We understand that postpartum is a time of recovery and rebuilding strength. But when you’ve experienced pregnancy loss, postpartum may not feel like it fits the season that you find yourself in at this moment, let alone returning to exercise after miscarriage or infant loss.
While you may not need or want to dial your fitness all the way back, being intentional in your return to exercise can help your body recover and help you maintain your long term fitness goals.
No matter whether you’ve experienced an early miscarriage, a stillbirth, or infant loss, your loss and your ability to get the recovery support you need matters.
Do you need to rehab your core and pelvic floor after a miscarriage or stillbirth?
Yes. If you’ve experienced a pregnancy, even if the pregnancy ended in loss, core and pelvic floor connection and a progressive return to fitness can help your body recover and help you maintain your long term fitness goals.
With pregnancy comes changes in the body, including hormones, postural adjustments, size of the uterus, constipation, etc. These changes can lead to an increase in pressure on the pelvic floor.
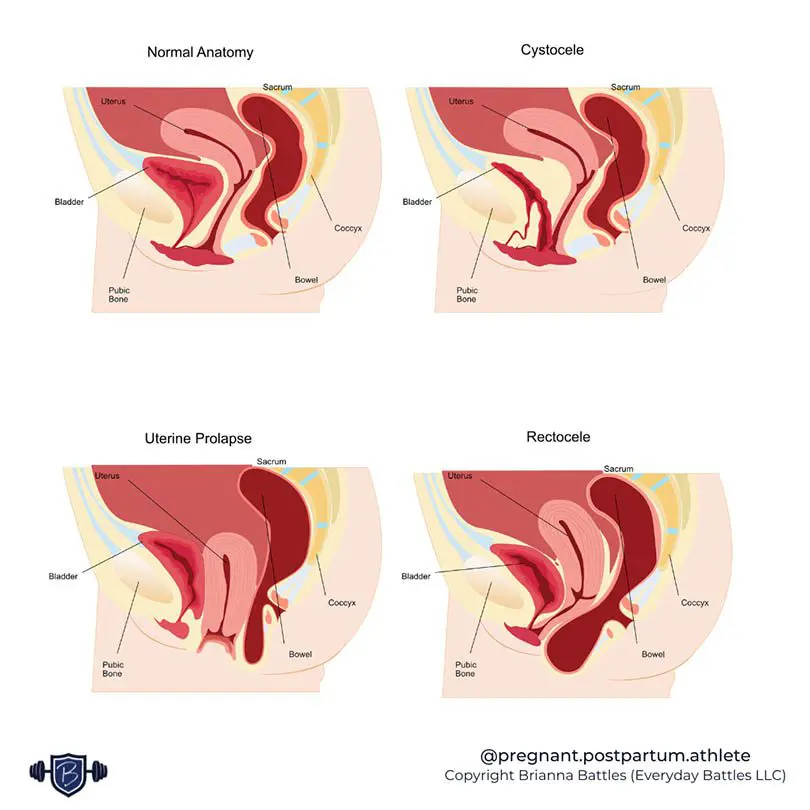
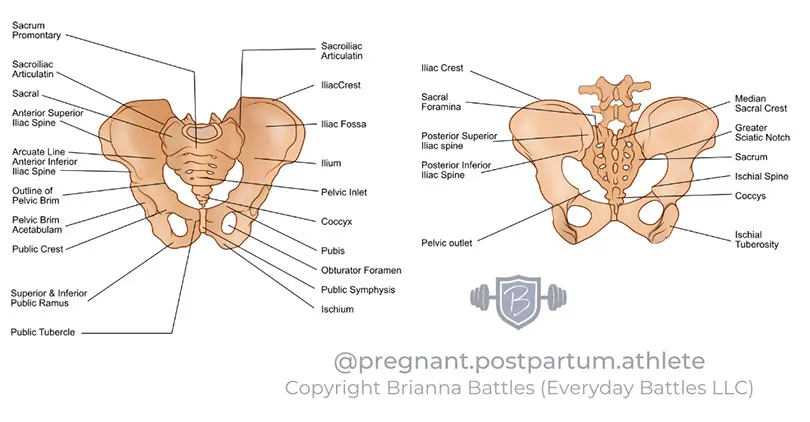
This increased pelvic floor pressure from pregnancy, even if only for a brief time period, can lead to an increased risk of core and pelvic floor disorders such as incontinence, pelvic pain, pelvic organ prolapse, or diastasis recti.
How to return to exercise after miscarriage vs a stillbirth?
There are more considerations for returning to fitness after pregnancy loss than simply knowing what trimester you were in when the loss happened.
Other things that can impact your recovery and return to fitness:
- What surgical interventions (if any) did you have? Ex: D&C, episiotomy, c-section, etc
- Did you have any complications? Ex: excess bleeding, high blood pressure, pelvic floor concerns
- Support and mental health. Ex: are you getting a decent amount of sleep, able to fuel your body with food, staying hydrated.
It’s not as simple as first, second, or third trimester. So how do you know what’s ok to do and what’s moving too fast? You can listen to your body, but when you don’t know what signs or symptoms to listen for or if you feel like your body betrayed you, that can be a difficult place to start.
Here’s a simple breakdown of common factors that you can take into consideration to figure out where you should start with your recovery and return to fitness.
- If your loss occurred during the first trimester, you had no medical complications, AND you had no medical intervention (outside of medication) – you can return to fitness close to where you left off. You may want to slow things down a tad, reduce the weights slightly, and add in some supportive core and pelvic floor work for best results.
- If your loss occurred during the second trimester, you had no medical complications, AND you had no medical intervention (outside of medication) – This is a time to take a slight step back. You can lift, but maybe you should try tempo and lighter weights instead of high intensity, high reps, and high load. Your body would likely benefit from mobility, core, and pelvic floor routines.
- If your loss occurred during the third trimester or later, OR you had medical complications, OR you needed surgical intervention – your return to fitness is going to look similar to a traditional postpartum path. Connecting to your core and pelvic floor, working on breath, balance, and a slow progressive return to strength will be key to helping your body through recovery.
Returning to exercise after miscarriage or infant loss isn’t a black and white event. You can speed things up or slow them down based on how you’re feeling in the moment and what you need in your recovery.
While you may not feel like you’re currently in a state of postpartum, being intentional in your return to exercise after pregnancy or infant loss can help your body recover and help reduce your risk of core and pelvic floor disorders and help you to maintain a lifetime of athleticism..
If you’ve experienced a pregnancy or infant loss, or are a coach helping your athlete through their loss, we’re here for you. You don’t have to go through your recovery on your own.
For more on how to support yourself or loved ones through pregnancy or infant loss, take a listen to Episode 12 of the Practice Brave Podcast where Brianna Battles and Casey Thomas-Hardesty discuss the spectrum of pregnancy loss and how to best support one another during this time.
Read More: Core and Pelvic Floor Basics